Wrap Network Health Insurance
The Network Options wrap plan allows out-of-area members to use participating health care facilities in their area at an in-network benefit level. First Health SelectCare The First HealthSelectCare Wrap covers all 49 states outside Wisconsin.

Pros Cons And Comparisons Hmo Ppo Cdhp Part 4 Hoopayz Best Health Insurance Health Insurance Healthcare Plan
The above arrangement falls apart if the PPO fails to market the health care providers services as in network or if the PPO makes the discounts available to Payers that are not part of the health care providers marketing plan that is if the PPO rents out the providers discount without the providers knowledge or consent.

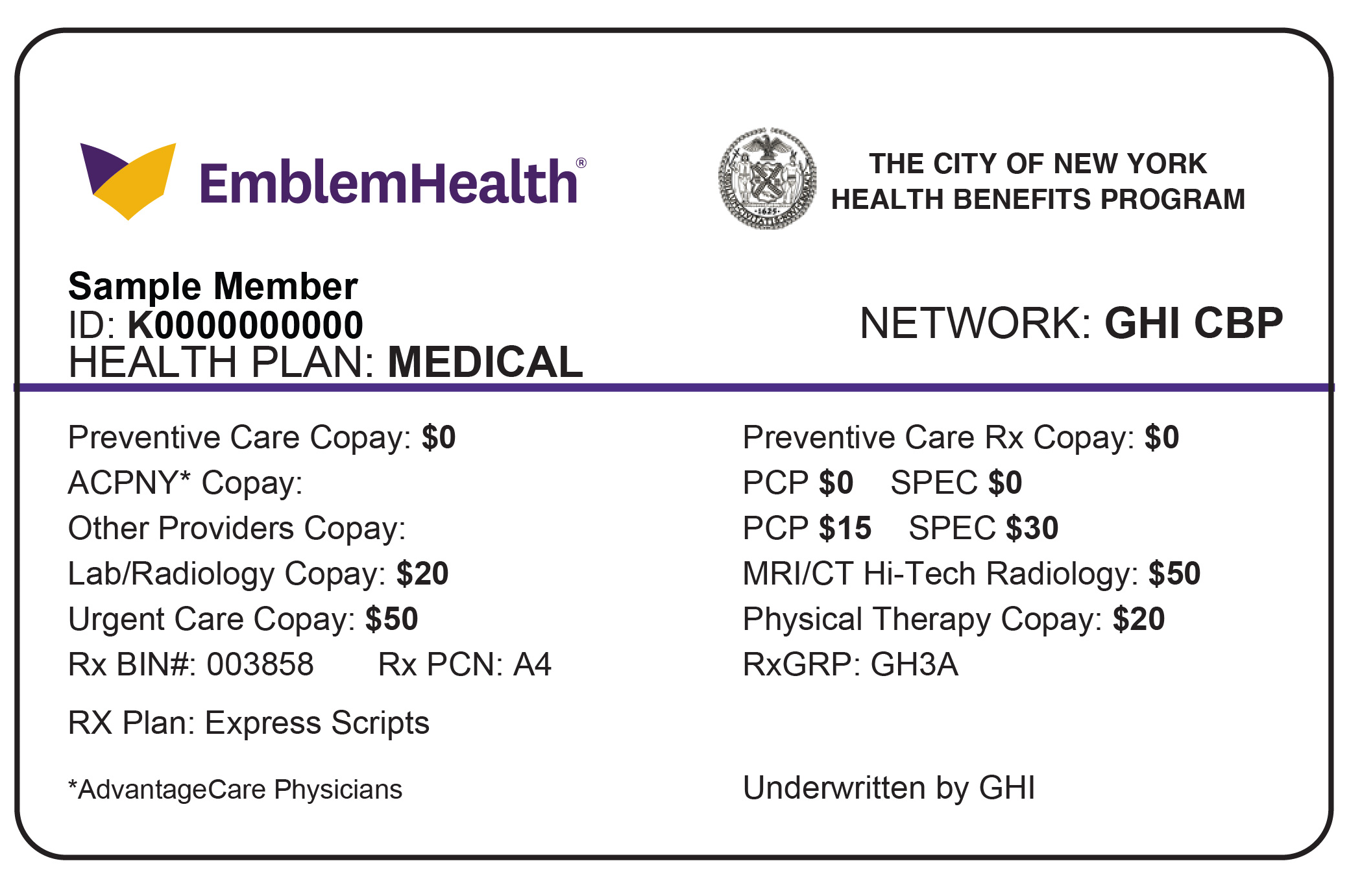
Wrap network health insurance. Dean Health Plan and Prevea360 have contracted with First Health to supply provider wrap network and Preferred Provider Organization PPO product network coverage effective July 1 2021. 2014 Wisconsin Physicians Service Insurance Corporation. For example if you have a dependent in college or are just traveling on vacation the wrap network is available outside of Ohio to ensure you get the benefits of staying in-network.
In network refers to providers or health care facilities that are part of a health plans network of providers with which it has negotiated a discount. MultiPlans PHCS Network is the only independently-contracted primary PPO network to have been Accredited by NCQA for credentialing a status weve held continuously since 2001. The approach generally works like this.
Since your insurance company will only pay a percentage of the reasonable and customary fee assuming your plan covers out-of-network. You can either choose an owner controlled insurance program OCIP or contractor controlled insurance program CCIP. When a wrap document is utilized the insurance policy or contract -.
Also wrap insurance policies give you the freedom to choose the best party to hold the coverage. To qualify for the Network Options wrap plan your company must have. Its useful to know your network and the providers in it to avoid high out-of-pocket costs.
It is also referred to as a wrap-around policy because it wraps. A wrap-around insurance program is a policy that provides punitive damages coverage for employment practices liability claims. Many plans sold in the health insurance marketplace have narrow networks but some employers offer them too.
Those members can receive care from out-of-network providers but will pay. More specifically a wrap document provides the information required by ERISA by incorporating or wrapping itself around the insurance policy or similar thirdparty contract. A wrap document is a drafting device used to supplement already-existing documentation.
You might consider a narrow network if you are young and healthy. If your organization has employees living outside the Network Health service area you may qualify to use Network Options wrap plan as part of your Network Health POS plan. Those members will not have coverage for services received by non-participating facilities except for emergency care.
First Health Network is one of the leading Preferred Provider Organization PPO networks in the United States. Insured individuals usually pay less when using an in-network provider because those networks provide services at lower cost to the insurance companies with which they have contracts. Blues Plans Wrap Insurance Products Around Value-Based Networks Jan 1 2017 Just as Blue Cross and Blue Shield plans are continuing to invest in value-based care models they also are wrapping insurance products around networks built on the foundations of these programs.
But since out-of-network providers dont have any contract with your insurance company those rules do not apply to them. The First HealthSelectCare Wrap for Individual Members NETWORK AT A GLANCE 1717 W. Wrap plans were developed as a strategy to help employers better manage their health insurance premium costs.
As a local health insurance carrier we understand that your health care needs may extend outside our 26-county service area. The Network Options wrap plan allows out-of-area members to use participating health care facilities in their area. To provide you with nationwide access to your PPO health plan benefits we partner with First Health Network.
In general an out-of-network provider may charge you whatever their billed rate is no matter what your health insurance company says is a reasonable and customary fee for that service. Employer XYZ currently has a group health plan with a 1000 deductible 80 co-insurance and office visit urgent care emergency room and prescription copayments. First Health has a robust provider network that will replace all.
PHCS Network is available in a variety of configurations including outside the plan service area to extend local HMO or PPO coverage nationally. Limited wraparound coverage allows an employer to provide certain employees dependents and retirees who are enrolled in some type of individual market coverage with overall coverage that is generally comparable to the coverage provided under the employers group health plan without eroding employer-sponsored coverage. The wrap network is designed to provide you with in-network coverage when you are outside of central Ohio.
You may not even realize you are in a narrow-network plan. The plan however desired to take better care of its employees and provide options aside from their narrow network so the plan elected to utilize Phia Unwrapped and chose 150 of Medicare as it allowable amount in an attempt to ensure that providers were paid only what the plan determined to be reasonable and customary healthcare fees.

Types Of Health Insurance Plans Health Insurance Plans Compare Health Insurance Types Of Health Insurance
What Does My Plan Cover Horizon Blue Cross Blue Shield Of New Jersey
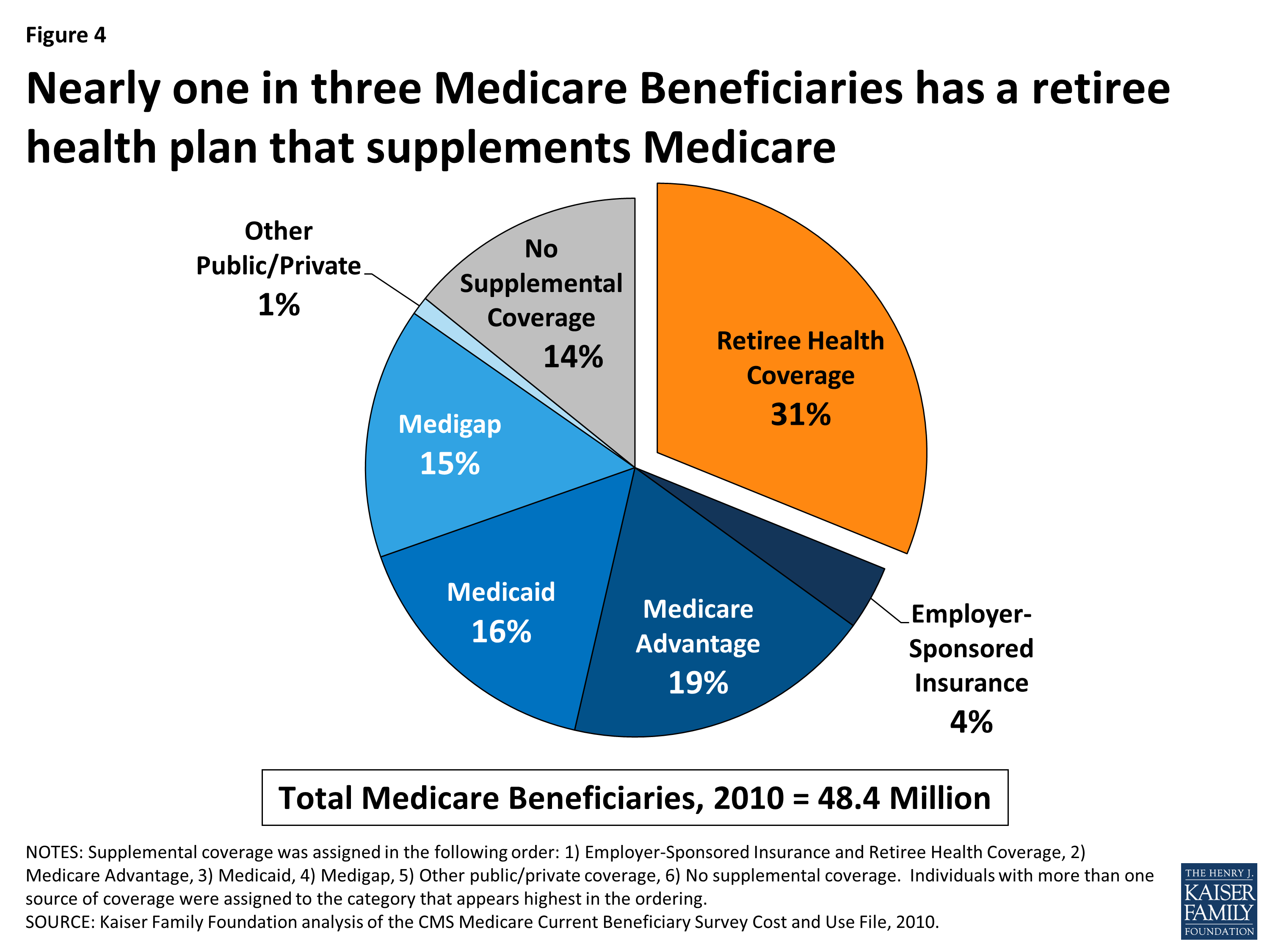
Retiree Health Benefits At The Crossroads Overview Of Health Benefits For Pre 65 And Medicare Eligible Retirees 8576 Kff